Yesterday I made a rare trip to London. The reason why I ventured back to the City of my birth, was a JDRF Discovery Day where the guest speaker was Dr Stephen Ponder. An American Diabetes doctor who also happens to have had Type 1 for nearly 50 years, diagnosed aged 9. He’s had a CGM for six years.
If you are wondering what is Sugar Surfing here is my definition (not Dr Ponder’s). It’s a lot more than this definition, but I wanted to put it into a sentence to help those who know nothing about it, get an idea of what it’s about:
It’s a proactive type of diabetes management that looks for certain instances in BG rises and falls and encourages the person to correct and manage those deviations now, to prevent hypos and hypers and get as steady BG as possible.
The Talk:
The talk started with the parent who kick started Dr Ponder coming to the UK. Elle Dormer had seen a friend on Facebook “like” his page (The Power Within) and looked at the page herself. She found it inspiring and helpful and decided to phone up JDRF and ask them to see if Dr Ponder could be brought over to the UK to give his talk. JDRF being the fabulous charity that they are, decided within 24 hours that they would like to go ahead and the rest is history. (Note, she did say that another well known diabetes charity in the UK (you know the one I mean!) took 7 months to do something after she contacted them.
The talk lasted a few hours, and had a lot of information so this is a looong post. I recommend you have a look at Dr Ponder’s website and if you have the money, buy the book. All the info on Sugar Surfing is on the website.
PLEASE NOTE: Sugar Surfing can be used for pumpers, non-pumpers and also those without CGMs. But it is easier with a CGM.
DISCLAIMER: These are my notes from the talk, and neither me or Dr Ponder are giving you diabetes care advice. It is a way to look at how you self-manage diabetes. I couldn’t get down everything that was discussed, but if you think it may be a method of D management for you or your child, please get the book, as there is SO much more to Sugar Surfing than what I have written here.
Dr Ponder (I’ll call him Dr P from now on) started posting his Sugar Surfing (SS) tips on his website and FB page. He was asked to compile them into a book. The book is now available but he never pushed it, and only mentioned it once I think. Dr P also put UK mmols on all his charts – very helpful as the US numbering of Blood Glucose (BG) confuses me totally.
Dr P pointed out early on that there are no good or bad BG numbers. There are just numbers, and it’s very important especially for parents to not burden our children by saying BGs are good or bad. It can have long term negative impacts on children.
What is Sugar Surfing?
Sugar surfing is a process not a recipe or formula. So if you are looking for one, you won’t get it. It’s about being proactive and living in the moment. If you see a dramatic change in a BG reading you act on it. Common sense really but not how many deal with their diabetes.
- It’s dynamic self management.
Dr P pointed out that most diabetes education is based on static care. i.e you change insulin doses based on past events. But SS is about management in the moment, it’s forward looking not backwards looking. If you see a dramatic change in BG then you act on it.
Static vs Dynamic Diabetes Care
Static D Care : actions are predetermined, there is minimal flexibility, outcomes don’t immediately affect actions, it’s easy to teach/learn.
Dynamic D Care (of which Sugar Surfing is one): actions are dependent on the situation/circumstance, flexible and adaptable, outcomes constantly influence subsequent actions, training is needed as well as ongoing reinforcement.
- SS is fuzzy logic. There is no formula. Every person is different. Be realistic – have low expectations to start. Sugar Surfing is a slow process.
- In SS, insulin dosing and giving insulin time to start working and see it effecting this is very important.
- In SS the correct basal rates are very important. So basal testing should be done to ensure correct basal rates.
(Note from me, I’ve never basal tested my son. He was 11 months old when diagnosed now 5 and it was impossible to basal test a baby. Even now, he is one of those children who cannot miss a meal. I know some do basal test, but I don’t think any parents should feel guilty or that they are doing the wrong thing by not basal testing. I have had the opportunity for impromptu basal testing where snacks and meals have been delayed due to various reasons, and I have to say most of the time the basal seemed correct).
Basic sugar surfing moves (things to look for) are: if you can’t read the text in the photo, click on the photo and it will give you a better quality picture.
- Basic microbolus (sorry don’t have a photo of this)
- Basic pivot:

Basic Pivot
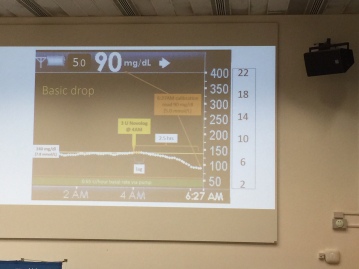
- Basic drop – 2-3 hrs insulin to work then BG drops after you need to correct
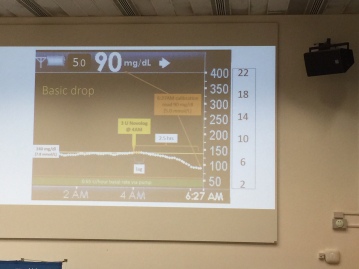
Basic Drop

Mini pivot

Mini Carb Pivot
- Insulin food mismatch and recovery:

Insulin mismatch and recovery
Remember, there is no formula in dealing with these occurrences, each individual person must learn how to deal with them themselves.
Sugar Surfing Mindset:
Let go of judging, feeling defective or broken, shame, fearing the future, isolation, pity, guilt
Embrace – acceptance, a sense of normalty, openness, enjoying the moment, teamwork, empowering/supporting, self-confidence
- Learn from your failures
- You can’t stop the waves but you can learn to surf
- Diabetes care is all about choices
- Diabetes care is best approached one day at a time.
SS requires the following: a working knowledge of principles/concepts, maintaining situational awareness, the ability to adjust to changing or shifting conditions
How to do it:
- Make ranges easy to achieve
- Aim high and wide at first
- Develop personal confidence
- Don’t hurry or rush it
- Lower/tighten target ranges VERY gradually
- As your skills improve, adjust your action thresholds
- Turnaround time: try and act sooner rather than leaving it
Pivoting is the key – known when to apply glucose or insulin pivot turn it around
So how do you do Sugar Surfing?
- Set high/low action limits on BGs
- Be mindful of rates of change it up or down arrows
- Consider recent current trends
Look at the BG stats and don’t miss an opportunity to act if you see any of the above. For example if BG is rising rapidly, give a correction – don’t wait for it to get even higher. If you do the correction earlier, the peak won’t be as high.
Traits of effective Sugar Surfers:

Principles of Sugar Surfing:

Calibrating CGMs tips:
- First day sensor can be erratic, calibrate on steady trend & in target range.
- Cal after large swings , after waking
Sugar Surfing Insulin timing and meal spikes:
- Insulin timing – take insulin before the meal 15/20 mins as this can prevent meal spikes, if you can, wait to eat until BG on graph starts to drop
- Stopping sugar spikes – a1cs show BG swings
- After meal control is very important to keep A1c below 7.5%
Micro dosing (Insulin and Glucose)
- CGM is needed for this aspect of SS. It is not the same as a full correction dose.
- Experiment with microbolusing
- Preempting – step in and stop a rise in BG.
- Dont look at the number look at the direction
- Micro carbing – to stop hypos
- Sometime you may need to correct your experiments – these are not failures
- You don’t need to wait to see the doc to tell you stuff – check out differences yourself
- Experiment with insulin and carbs
- Aim small miss small
Other tips:
- Develop skills at night targets first
- Practice practice practice
- Prior skills must be masetered first
MDI iChains: (nothing to do with Apple!) Specially for people on injections, not pumping
This is where you inject multiple times for difficult foods etc. It’s the equivalent of a square/extended bolus on a pump
- Learn your own insulin duration to forge ichains
- Managing slow trends – correct at pivot – be patient
- Don’t miss an opportunity to correct an out of range BG
- Preempt meal spikes
Engine Braking:(stopping a hypo)
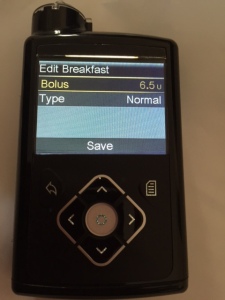
Turn off basal to try to stop a hypo ( note from me, the Medtronic 640G does this) or zero temp basal.
Final note from me: I was quite pleased to see that I was already doing some Sugar Surfing to a small degree. I don’t ever claim to know it all, and there is much I can use from this. But I think it’s helped me the most to see that it’s ok to make adjustments through the day, every day. I was constantly striving for that magic basal/bolus/correction factor and actually I can now stop stressing about that and go with the flow more – use the pump + CGM to it’s fullest and not feel I’m failing. Or at least not beat myself up about adjusting things. So that has been priceless. Thank you Dr P.
I used to think I was fire-fighting, I was actually Sugar Surfing.